Suicide rates increased by 25% across the United States over nearly two decades ending in 2016, according to research published Thursday by the US Centers for Disease Control and Prevention. Twenty-five states experienced a rise in suicides by more than 30%, the government report finds.
More than half of those who died by suicide had not been diagnosed with a mental health condition, said Dr. Anne Schuchat, principal deputy director of the CDC.
“These findings are disturbing. Suicide is one of the top 10 causes of death in the US right now, and it’s one of three causes that is actually increasing recently, so we do consider it a public health problem — and something that is all around us,” Schuchat said. The other two top 10 causes of death that are on the rise are Alzheimer’s disease and drug overdoses, she noted.
In 2016 alone, about 45,000 lives were lost to suicide.
“Our data show that the problem is getting worse,” Schuchat said.
Increases in 49 states
Using data from the National Vital Statistics System for 50 states and the District of Columbia, CDC researchers analyzed suicide rates for people 10 and older from 1999 through 2016.
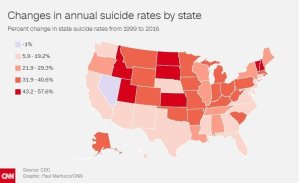
Overall, the US experienced a 25% rise in the rate of suicides during that period, with individual states ranging from a 6% increase in Delaware to a nearly 58% increase in North Dakota, the researchers say.
All states except Nevada experienced an increase; although Nevada showed a 1% decrease in suicide, the state’s suicide rate was still high, ranging between 21 and 23 suicides for every 100,000 people through the years studied, the researchers say.
Suicide rates were four times greater in the highest state compared with the lowest when calculated on an annual basis during the most recent time period, 2014 to 2016.
Montana experienced about 29 suicides for every 100,000 people — the highest in the nation — compared with about seven people out of every 100,000 in the District of Columbia — the lowest. As a whole, the nation saw 15 people dying by suicide for every 100,000 in 2016.
“The most common method was firearm, followed by hanging or suffocation, followed by poisoning,” Schuchat said. “Opioids were present in 31% of individuals who died by poisoning.” She added that intentionality is difficult to determine in cases in which a person dies by overdose.
Deborah Stone, lead author of the study and a behavioral scientist at the CDC, said Thursday, “We typically see that firearms make up about half of all suicides, and that tends to be pretty consistent.”
Schuchat noted that the researchers “focused in on 27 states where we have extensive data from the death investigations to try to understand the factors or circumstances leading up to suicide.”
These data, derived from the National Violent Death Reporting System, showed that 54% of those who committed suicide in 2015 did not have a known mental health condition. Digging deeper, the researchers found that several circumstances, including the loss of (or problems in) a relationship, were more likely to trigger a suicide among those who did not have a mental health condition.
Regions and demographic groups were also compared.
Economic factors behind suicide
The Western area trend of high increases in suicide rates could be related to the fact that people in rural areas have less access to services as they more slowly benefit from the economic recovery than other parts of the nation, she said.
“We don’t have all the answers. There may be several, but we knew that economic factors can increase the risk of suicide and that limited access to care, behavioral and social services may also increase the risk of suicide,” Schuchat said.
Recent government reports have highlighted rising rates of suicide among women. “The percent increase was higher in women, but it’s important to say that men have a three to five times higher rate than women,” Schuchat said. The rising suicide rate for women, then, is “increasing but at a much, much lower level” than for men.
Veterans are also “overrepresented” in the report, she said.
“Veterans made up about 18% of adult suicides but represent about 8.5% of the US adult population,” Schuchat said, noting that not all veterans who died by suicide were recent veterans. Still, the researchers found a 10% higher risk of suicide among people who had served in the military.
Middle-age adults had the highest increase.
“This is a very important population right now in terms of national statistics,” Schuchat said, noting the high rates of drug overdose in this group as well as “deaths of despair” described in social science literature. She believes this group may have been hardest-hit by the economic downturn, but she added that unknown factors probably contributed.
“We think a key message is, there’s not just one group; many are at risk,” Schuchat said.
Whether or not they had a mental health condition, most people who died by suicide had experienced “one or more factors that may have contributed, including a relationship problem, a crisis in the recent couple weeks and problematic substance abuse,” she said.
‘Alarming’
K. Bryant Smalley, a professor of community medicine and psychiatry at the Mercer University School of Medicine, described the mental health care challenges experienced by patients in rural areas as the “three A’s”: availability, accessibility and acceptability of care.
Smalley, who was not involved in the new research, pointed out that about 85% of federally designated mental health professional shortage areas are rural.
“Due to higher poverty rates, higher likelihood of hourly pay and productivity-based labor, and lack of transportation infrastructure, mental health services are often not accessible even if they are available in a rural community — that is, even though it is there, many people either cannot get to it or cannot afford (either directly or indirectly) to go,” he said.
Add to that, rural areas have very high levels of stigma surrounding mental health services. “Rural residents face lower levels of anonymity in seeking services due to the close-knit nature of rural communities,” Smalley said. The possibility of “someone seeing your car parked at the only psychologist’s office” means rural residents are less likely to seek care when needed.
Dr. Sandro Galea, dean and Robert A. Knox Professor at the Boston University School of Public Health, said the National Vital Statistics System is the “best system we have of keeping records in the country.” Galea, who was not involved in the new study, added that for this reason, the new research should be taken “very seriously.”
“There have been previous reports recently that have shown suicide is one of the major contributors to a decrease in life expectancy in this country, which makes it even more alarming,” he said.
“The paper makes a clear case, correctly, about the fact that there is no one cause for suicide,” he said, adding that “availability of means” makes death possible.
“A lot of suicide is a one-time effort, so having guns available, for example, makes one more likely to complete suicide, but that in and of itself is not an explanation for why suicide is going up,” Galea said.
“CDC data shows that suicide happens to everybody,” he said. “Social and life and economic stressors are the ones that create the conditions for suicides to happen.”
If you feel extreme distress, you can call 1-800-273-8255, the National Suicide Prevention Lifeline, to speak with someone who will provide free and confidential support 24 hours a day, seven days a week. If you want to learn how to help someone in crisis, you can call the same number.
The CDC also recommends its own policies, programs and practices for prevention.
Shuchat said there are simple steps anyone can take to help someone at risk. “Beginning a conversation, helping keep them safe, helping them connect and then follow up with them,” she said. “We don’t think every single suicide can be prevented, but many are preventable.”





















